Feeding Tube Tips for Heading Back to School
Feeding Tube Tips for Heading Back to School
The start of a new school year is an exciting time for all families, but sending your child with a feeding tube to school for the first time can be nerve-wracking for both parents and kids. That’s why we put together our tips for tube feeding at school, particularly when using our meals or a home blended diet. With a little preparation and organization, tube feeding at school doesn’t have to be that different from feeding at home.
Before School Starts
Most schools will require a doctor’s note or doctor instructions to feed your child during the school day. Including your child’s feeding plan in their IEP and 504 plans is also important. Offer to train the person who will be feeding your child at school, whether that is the school nurse, an aide, or someone else. Also make sure at least two people are trained to feed your child in case the main person is ever unavailable. The Feeding Tube Awareness Foundation has a free School Training Presentation designed to train school nurses, teachers, aides, and other school staff about tube feeding. Be specific about volume and feeding times in the feeding schedule you have on file with the school. If your child uses a pump, tell school staff how to deal with any pump alarms that might happen. Many schools will have a specific protocol for how they handle a feeding tube that comes out during the school day, so make sure you know your specific school’s policy, including if you can send an emergency kit to replace a feeding tube at school.

Preparing for the First Day
Ahead of your child’s first day of school, make sure you label everything you’re sending, from syringes to insulated bags to pump bags and backpacks (if used). If your child is using Real Food Blends meals, you can send them to school without an ice pack or cooler, but make sure the school is aware that any leftovers need to be refrigerated within 2 hours of opening the pouch. If the school allows you to send food ahead of time, you can send Real Food Blends meals one week at a time or more since they are shelf stable for 3 years from the date of manufacturing. If you bolus feed and are sending blends from home, or just want to save time during the school day, mom Kara recommends sending prefilled syringes. “I prefill syringes and cap them for the nurse daily. Then I put them in a one-gallon Ziplock bag with a primed extension. Makes it easier for the nurse and in turn a quicker experience for our son!” Just remember with this option, whether you’re using home blends or Real Food Blends, to send the pre-filled syringes in a cooler/insulated bag with ice packs and make sure the syringes are refrigerated at school until they are ready to be used.
Helping Your Student Adjust
While you may be nervous about sending your child to school for the first time with a feeding tube, remember that your child might be nervous, too! If this is your child’s first overall experience at school, they may have questions about their new schedule and who will be helping them throughout the day. Make sure to walk your child through their schedule and explain to them where they need to go for tube feedings and who will be helping them. Don’t be afraid to adjust your child’s feeding schedule during the school year, too. Being nervous about a new routine might mean your child won’t be able to take the same volume at school—consider making lunch smaller and incorporating a before or after lunch snack into their school feeding schedule or an after school snack at home. When possible, we always encourage those using Real Food Blends to use a mealtime schedule just like those who eat orally, which often includes a snack in addition to breakfast, lunch, and dinner. We’re just talking about food, after all!
If your child previously ate orally, they may be nervous about answering questions about their feeding tube at school and how lunchtime will be different. Giving a presentation to your child’s class about tube feeding at the beginning of the school year can be a great way to alleviate some of these worries for your child and make his or her classmates feel more at ease with feeding tubes. Feeding Raya has a great example of a presentation her kids gave to their classes about their younger sister with a feeding tube. For preschool or kindergarten classes, reading My Belly Has Two Buttons to the class is a great option as well.
If anyone at your child’s school has questions about Real Food Blends, our new RD Hub is a great resource or you’re welcome to direct them to call us at 888-484-9495. You can also reach out to us via our Facebook page. The Feeding Tube Awareness Foundation also has a wealth of general tube feeding information, especially for those new to tube feeding. From all of us at Real Food Blends, we wish you and your child a fantastic school year!
The Story Behind Our Meals

The Story Behind Our Meals
Clean Ingredients, Clean Labels
Whether you’re new to Real Food Blends or have been using (or recommending) our meals for years, you may not know why our meals are the way they are. Although we started with three meals and now have six, we’ve stayed with the same philosophy from the beginning—that simple variety is best. If you’re an RD, you may recognize that our meals are based on the USDA’s Choose Your Plate guidelines and each includes a fruit, vegetable, whole grain, and protein; you only need to add a side of dairy to have a government-approved meal.
Meals, Not a Formula
What that means is that we have 5-7 ingredients in each of our meals on purpose—we believe whole food ingredients are best (the less processed, the better.) There’s no need to spend hours combing over our ingredient list to see if there’s something hidden in there that might interact with a medication or that might be a different form of an ingredient you or your loved one can’t tolerate—our ingredient lists will always be short, simple, and easy to read because we ONLY include real food ingredients in our meals.
When choosing the specific ingredients, we always include a full serving of fruits and vegetables in every meal along with a whole grain, lean protein, and healthy fat. Sounds a lot like what most doctors and dietitians recommend to their oral eating patients, right?! As long as the digestive system is still intact, what we all know about good nutrition still applies to those with feeding tubes. Does a vegetable become less good-for-you if it goes through a feeding tube? People with feeding tubes can benefit from healthy, real foods just like oral eaters—they just need a different way of getting those foods into their stomachs. All of our ingredients are consciously sourced as well, including:
- Grass-fed beef
- Wild-caught salmon from the Pacific Northwest
- Only US-raised chicken and eggs
- Certified Gluten-free oats*
That being said, our ingredients are not organic, and that was also something we chose on purpose. We understand that organic is very important to some people, but we made the decision to focus on real, whole foods while keeping costs down so that our meals are affordable for people paying out of pocket and to make sure our meals are easily available to those with insurance coverage. The high heat process that our meals go through to make them shelf stable (which is the same process many food products go through to make them shelf stable) also can minimize any benefits that might be gained from using organic ingredients. Studies in general have been mixed as to the actual levels of increased nutrients in organic foods and many experts agree that WHAT you eat is more important than whether you choose organic versus conventional. If organic is important to you, we would highly encourage you to work with your dietitian and blend fresh organic food versus any organic tube-feeding formula that’s shelf-stable.
Why 6?
So now you know why we have simple, consciously-sourced, whole food ingredients in all six of our meals, but you might not know WHY we have six different meals. After all, in the past formulas for feeding tubes have been designed to have someone use the same formula all day, every day. That just didn’t make sense to us. People who don’t have a feeding tube are told to eat a wide variety of healthy foods every day, so why shouldn’t people with feeding tubes be given the same recommendations? Here’s what Alissa Rumsey, MS, RD, CDN, CSCS, a clinical dietitian at one of New York’s largest hospitals, has to say about that.
“Think about people who eat by mouth. No one eats the same meal and ingredients over and over again, every single meal, every single day. As a dietitian, I would never recommend that, even if the patient was taking a multi-vitamin every day. So why are we recommending it to people on tube feeds? Nutritional variety is just as important –if not moreso- as nutritionally complete.”
What’s NOT In There
Now that we’ve talked about what IS in our meals, what about what ISN’T? Like added synthetic vitamins. We know some medical professionals focus on nutritionally complete products for their enteral patients (read more about the concept of nutritionally complete), but we kept added synthetic vitamins and minerals out of our meals for a variety of reasons.
- Synthetic vitamins can cause nausea and leave a nasty after-taste when burped.
- Not all people with a feeding tube need the same amounts of these vitamins, given their underlying conditions. It’s not unusual for someone to need a low-sodium diet, low potassium, or have other unique nutritional needs that are not one-size-fits-all.
- Potential for medication interactions.
- Potential to greatly exceed RDIs.
After all, once you put vitamins in, you can’t take them out. Everyone has individual nutrition needs, different medications that can impact certain vitamin and mineral levels, and different health considerations. A child with cystic fibrosis isn’t going to have the same nutritional needs as an adult who suffered a traumatic brain injury. Consult your medical team for your specific nutritional needs, but in general, if you’re using our meals as a sole source of nutrition, we just recommend adding a daily multivitamin and a dash of salt once a day (our meals have no added salt, either!).

We hope this sheds some light on the story behind the creation of our meals, especially for those who are newer to Real Food Blends. No matter what, know that our meals will always contain nothing but simple, whole food ingredients that provide real food and nutritional variety for people with feeding tubes. Our co-founders, Tony and Julie Bombacino, founded Real Food Blends after seeing their own tube-fed son improve so drastically on a blended diet—we will always only offer meals that we’re proud of and contain ingredients we would feed our own families.
Interested in trying Real Food Blends for the first time? Our Trial 6-Pack is a great place to start as it has one of each of our five meals!
*Our meals are not certified as gluten free, but do not contain any gluten ingredients. They are produced in a gluten handling facility.
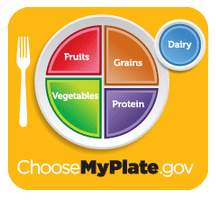
Transitioning Away From Overnight Feeds
Transitioning Away From Overnight Feeds
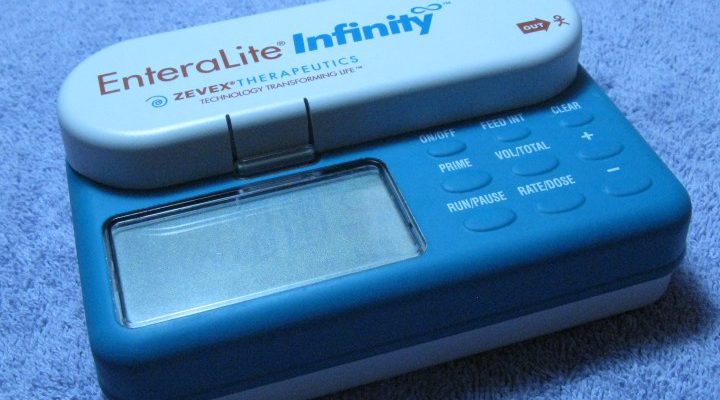
Almost daily here at Real Food Blends, we get asked if our meals can be used for overnight feeds or if they can put the meals on ice to feed overnight or if the meals can go through a pump to be fed overnight….
Wait, what? Eating while sleeping??
 When you start to think in terms of MEALS and less in terms of FEEDS, feeding overnight starts to sound a little strange. Oral eaters don’t have to wake up every night to eat, right? And many would argue that our digestive systems need to rest at night.
When you start to think in terms of MEALS and less in terms of FEEDS, feeding overnight starts to sound a little strange. Oral eaters don’t have to wake up every night to eat, right? And many would argue that our digestive systems need to rest at night.
For some people, the idea of NOT feeding overnight is super scary – “How will we ever hit our calorie goal? We can’t get that volume amount in during the day!” These questions are almost always from those who are 100% formula fed. (Requiring overnight feeds can be a sign of formula intolerance however some conditions require so many extra calories that overnight feeds are a must – cystic fibrosis is one that comes to mind immediately – but we’re speaking in generalities here!)
To our knowledge no one has really studied this, but in our experiences and from a lot of anecdotal “evidence,” overnight feedings can lead to volume intolerance during the day (especially in the morning – who’d want to eat breakfast after eating all night?), increased risk of reflux/aspiration (usually due to not being upright for eating, you try to eat laying down and see how you feel!), disrupted sleep, and scary episodes of vomiting/choking.
If the only reason you or the person in your life with a feeding tube requires overnight feeds is to hit a calorie goal, read on:
Real Food
The first tip we’d offer is to introduce real food into the tube-feeding diet. Real Food Blends meals are thicker than formula in part to provide more nutrition and calories per ounce, making it easier to meet your calorie needs in a shorter amount of time. (There’s also some evidence that volume tolerances increase with real food.) Real food can be used alone or with formula and transitioning someone who has been exclusively on formula for any amount of time should be done slowly (read more about how to transition from formula to a real food diet. See also: Is Real Food Right For Me?)
Normal Mealtime Schedule
We like having a goal to move to a normal mealtime schedule – breakfast, lunch, snack, dinner – when transitioning to real food. Again, if you think about this from an evolutionary perspective, this is how humans have been eating for ages! This transition should be done slowly and over time—you may want to gradually increase the amount of food given during the day and slowly decrease the amount of formula given overnight. The more calories you can get in during the day, the fewer you’ll have to give during an overnight feed, with the goal of getting all your necessary calories in during waking hours (like humans have been doing for ages!)
Think Midnight Snack
While making this transition, giving a small bolus feeding at night instead of a continuous overnight feed might be helpful. Think of it more as a “midnight snack”—the stomach still gets to rest during most of the night and you have another opportunity to get some extra calories in while you’re transitioning away from overnight feeds.
Volume
If volume is a concern, we suggest going slow and adding additional volume in small increments during the day, perhaps starting out with just an additional half an ounce per meal. Many people have found that giving free water prior to a meal can help increase volume tolerance as well—make sure to discuss hydration needs with your medical team. See also: Tube Feeding and Volume Intolerance
“I have had my feeding tube for almost 4 years now. I had tried multiple different formulas that were just marking me very sick so I would just go without food. I tried just making home blends but was struggling to balance the vitamins and calories so I was still getting sick. I tried Real Food Blends and the difference was night and day no more reflux no more heart burn.”
- RFB customer Kim Inslee-Pomerleau
What’s your experience with overnight feeds been? Have you been able to successfully transition off the tube at night? We’d love to here your feedback here or on Facebook.
*****
As always, please talk to your doctors before making any changes to your tube-feeding diet. This is not to be considered medical advice.
The Facts About “Nutritionally Complete”

The Facts About “Nutritionally Complete”
This is a special guest blog post by Alissa Rumsey MS, RD, CDN, CSCS
As a clinical dietitian at one of New York’s largest hospitals I worked with thousands of patients with a feeding tube. In the hospital, my go-to tube feed source was a typical commercial enteral formula. I was taught that these formulas were “nutritionally complete” and often shared this with my patients and families when I taught them about tube feeding.
Most dietitians and healthcare professionals in the tube feeding world use the term nutritionally complete just as I did, without a second thought. But once I began working with people who use real food in their tube, I realized that most people don’t fully understand this idea of nutritionally complete and believe it to be more important than it is. Here’s why I don’t prescribe to the concept of a “nutritionally complete” formula anymore.
What does nutritionally complete actually mean?
A tube feeding formula is considered nutritionally complete if: it provides 100 percent of the recommend values of carbohydrates, protein, fat, vitamins, and minerals and can be used on its own as a sole source of nutrition. While it may be easy to have an all-in-one formula that you can just open and pour, and that we as medical professionals can recommend knowing the patient is receiving everything he or she technically requires to live, this doesn’t necessarily mean these formulas are best, especially for long-term use.
Most people placed onto feeding tubes are trying to gain weight, meaning they need more calories from proteins, fats, and carbohydrates than someone of a similar age. The RDIs were created for healthy people and the population as a whole, which is generally not underweight. If a child is put onto a 1500 daily calorie plan of a typical pediatric enteral formula, they will be getting up to 150% of certain vitamins and minerals, which may be too much for many children. This is the biggest issue with “nutritionally complete”: Once the vitamins and minerals are in a formula, there is no way to take them out.
Aside from unintentionally prescribing higher-than-recommended levels of RDIs, what if the patient is on a medication that interacts with certain vitamins and minerals? What if your blood level of a certain mineral is too high? There’s no way to adjust the nutrients in the pre-made “nutritionally complete” formulas. Compare this to using a product like Real Food Blends that doesn’t contain any added vitamins and minerals. You can easily add the desired amount of vitamins and minerals to your blended meal, providing more or less of different nutrients based on your individual needs.
Another important point to think about is synthetic versus food-derived vitamins and minerals. Fruits, vegetables, and whole grains are full of nutrients and phytochemicals that can improve vitamin and mineral bioavailability and absorption. While the vitamins may be chemically identical, there is some research to support that the synthetic forms, like those found in commercial formulas, are not as well absorbed and utilized as the form found in whole foods.
Nutritionally Complete vs. Nutritional Variety
Nutrition is a complicated science. We have only scratched the surface of understanding how our bodies use nutrients and which of those are essential. The nutritionally complete formulas assume that we know all there is to know about what makes something nutritionally complete, when in reality we don’t. Just because something is thought of as nutritionally complete does not mean it is the perfect food. As Eric Aadhaar O’Gorman said in the book Complete Tubefeeding, “Commercial formula companies do a good job of trying, but can never replicate the sort of spread of nutrients that a varied diet gives us.”
Think about people who eat by mouth. No one eats the same meal and ingredients over and over again, every single meal, every single day. As a dietitian, I would never recommend that, even if the patient was taking a multi-vitamin everyday. So why are we recommending it to people on tube feeds? Nutritional variety is just as important –if not moreso- as nutritionally complete.
With my clients who eat by mouth, I talk non-stop about the importance of a varied diet. The larger the variety of foods consumed, the more variety of vitamins, minerals, antioxidants, and phytochemicals you get. Think about the wide variety of food that people eat from day to day. Now, imagine “eating” these same foods via a feeding tube. From a quality of life perspective, there is no beating real food. While someone fed through a tube can’t necessarily taste all the food, they can still smell it, burp, and get a sense of the flavors. I have one patient who desperately missed his morning cup of coffee. After getting the ok from his doctor, we started giving him some coffee through his PEG. As his wife was preparing his breakfast blend, he would sit holding the cup of coffee and enjoy the scent and smells. Once he got his breakfast, the coffee would be cooled enough, and he would give it through his PEG. The feeding experience becomes more normal when you incorporate real foods.
There are other benefits to real food. Many people have trouble tolerating commercial formulas and have GI issues like nausea, bloating, vomiting, and diarrhea. As Julie Bombacino, co-founder and CEO of Real Food Blends (and the mom of a tubie), said to me once, “If they’re pooping or puking or refusing feeds, they’re not getting ‘complete nutrition’!”
All of my patients have an improvement in gastrointestinal function when they start using real foods. Their volume tolerance improves too, and they often have no trouble taking in larger quantities of food, despite having issues with similar amounts of formula. One patient of mine was getting in less than half the calories he needed because every time he gave himself a commercial formula, he had severe nausea and reflux. Once we transitioned him to blended tube feeds using real food, his symptoms completely went away and he was able to get all the nutrients he needed.
Using Real Food Blends as your primary source of nutrition? Most people should also consider taking an age appropriate multivitamin and calcium and sodium supplements daily.
Here is the complete nutritional information for Real Food Blends meals.
Moving Beyond “Nutritionally Complete”
Some dietitians and health practitioners get caught up in the idea of developing nutritionally complete blenderized tube feeds, thinking that it is obscure and complicated. I get it; I once felt the same way. Commercial formulas seem so straightforward: calculate a total volume of formula and you know exactly how many calories, macronutrients, vitamins, and minerals that person is getting. But in reality, it’s not much more complicated with real food. Think about how you construct meals for individuals who are eating by mouth. Do you worry that they aren’t going to get all the vitamins and minerals they need? No, because you recommend a varied diet with a variety of foods from different food groups and probably a good quality, age-appropriate multivitamin for some people. The same goes for tube-fed individuals. You can plan balanced, blended tube feeds for those that want to make homemade blends, and Real Food Blends can offer easy access to whole foods as well.
It’s time to think beyond nutritionally complete and stop using commercial formulas just because it’s what we’ve always done and it checks all the boxes for complete nutrition on a piece of paper. I challenge you to think about feeding people with feeding tubes similarly to those who eat by mouth. We need to balance how easy it is to prescribe commercial formulas with remembering how people actually eat and SHOULD eat (hint: not the same thing for every meal every day, but a wide variety of vegetables, fruits, whole grains, seafood, meats, and more). People with feeding tubes experience many of the same feelings we as oral eaters do – the smell of food, the taste of food, feeling of being full or bloated after a big meal – and their bodies deserve to reap the benefits a wide variety of whole foods can offer.

Alissa Rumsey MS, RD, CDN, CSCS is a nationally recognized Registered Dietitian based in New York City. While working in the intensive care unit at New York-Presbyterian Hospital, Alissa quickly saw the long-term effects that poor nutrition and physical inactivity could have on the body. After working for six years with critically ill adults, she developed Alissa Rumsey Nutrition & Wellness Consulting to help others improve their health and wellbeing. She consults with a variety of home tube feeders to help optimize their tube feed diet with whole, real foods. For more information about Alissa, visit blenderizeddietrd.com and alissarumsey.com.
Tube Feeding and Volume Intolerance

Tube Feeding and Volume Intolerance
Volume intolerance refers to the inability for a person with a feeding tube to handle a typical tube feed in a normal period of time. The volume and time frame can vary by age, caloric needs, etc. There’s not really a threshold for this. If you compare how long it takes for a person who eats orally to finish a meal versus how long it takes for someone on a feeding tube to finish their meal, this can give you context of volume tolerance/intolerance. If you are tube-fed and need to have your full formula feed dripped in slowly over a long period of time (anything over an hour), you could be considered volume intolerant.
Before I had a child with a feeding tube, I had never heard this term. Us oral eaters don’t talk about being “volume intolerant” – we just stop eating before we get too full! But in the tube-feeding world, this term is often cited as a side effect of tube feeding. The typical ways to deal with it? Slow down the feeds, feed smaller meals more often or maybe even switch formulas. “Volume intolerance” is how many people with a feeding tube end up on a slow drip of formula over the course of a day or on continuous or overnight feeds in order to get the prescribed calories in each day.
One of the anecdotal things we often hear in the tube-feeding community is that ‘volume tolerance’ improves with real food. Magic elixir? Hardly … think of it this way. If you were a typical eating child, the photo to the left is an example of what the USDA recommends you have for lunch (see more details at choosemyplate.gov). So why do so many people with feeding tubes – even adults – have a hard time handling 8 ounces of formula in a 20-30 minute period? That’s volume (or formula) intolerance.
How to improve volume tolerance for tube-feeding
“Overall, we have found greater volume tolerance and improvements in reflux and constipation when switching from commercial formulas to blenderized tube feedings.” – The Use of Blenderized Tubefeeding, Novak / Wilson
“It is a well-known fact that most tubes tolerate far higher volumes of food than formula, and much of this is down to the feel of the food; how our bodies communicate with us about the appropriateness of our nutritional needs.” – Complete Tubefeeding, O’Gorman
Switching from an enteral formula-only diet to real food through the feeding tube can help some people with volume intolerance issues. Real Food Blends meals are intentionally thicker than traditional formulas partly to provide more nutrition / calories per ounce. Each pouch yields an 8 ounce serving at about 40 calories per ounce. An 8 ounce serving of our 100% real food meals will provide approximately 80 more calories per serving than a traditional enteral formula so those people with volume issues can take in more calories in the same amount of food. We have tips for transitioning to our meals from a formula-only diet here, and usually recommend that you keep the same volume over the same amount of time that you would feed formula to start.
Once you have established that our meals are working well for you, you can begin to experiment with volume changes. Moving to a more normal mealtime schedule (breakfast, lunch, snack and dinner) is possible and preferable for many people with a feeding tube!
Time or Volume?
It’s important to think of volume tolerance in terms of goals. Are you trying to shorten the amount of feeding time per meal/day, or is it more important to you to increase the amount of food at each meal? We suggest only trying to do one or the other to start. Most people, especially kids, can’t just go to this right away:
If you are having 8 ounces over a 45-minute period, your first goal may be to shorten the feeding time to 40 minutes. If tolerated well, then move down to 35 minutes. This is all trial and error but slowly shifting to a normal meal timeframe can free up a lot more time in your day (within reason! Some people have their meals in a few minutes, some will need 20-30 minutes. Both of these are pretty normal – we all know that some people are fast, or slow, oral eaters!) If you are caring for someone who is nonverbal or unable to communicate, you’ll need to look for other clues as to how this is being tolerated:
“Children with a feeding tube often discover other physical ways of saying ‘no.’ Gagging and retching may be the response of a child who is beginning to feel uncomfortable. The child may become physically tense and emotionally stressed from the fear of getting too much food or feeling sick. Children who increase tension on the abdomen, cry or develop irregular breathing patterns often find their tension will slow down or stop the flow of the formula. Their increased agitation during the meal can limit the amount of formula they receive, but it also increased gastrointestinal discomfort.” – Suzanne Evans Morris, Ph.D, CCC, “Mealtime Communication and Homemade Blended Formulas” from Homemade Blended Formula Handbook
If your first goal is to increase the amount of food / calories being served at each meal, again, we suggest going slow. Using our same example above of an 8 ounce serving over 45 minutes, you may want to start at adding a half ounce to each meal to see how that’s being tolerated. Over 3-4 meals a day, that’s another 120 or so calories, which can add up!
Again, if the person with a feeding tube is unable to communicate, you’ll need to look for other indications that they are full / that the increased volume is – or isn’t – being handled well. Additionally, you may find that the digestive system speeds up with the introduction of real food and will need to look for hunger clues BEFORE the next scheduled meal. Some people find that checking residuals can help determine if the person is ready for the next meal / more food / volume.

” We usually struggle to get 8 ozs in of formula because she is too full but she was able to take the whole packet without a peep!” Peyton’s mom, Tracy, shared on our Facebook page
Free Water
One of the tips that often seems counter-intuitive to increasing volume tolerance is increasing the free water given. Free water refers to water given through the tube outside of what’s in a formula or blend. (Again, us oral eaters would call this a drink of water!)
“Many parents and therapists have found that offering a water bolus 30 minutes prior to the tube meal supports both the greater fluid needs of a child receiving thicker food-based formulas and improves the child’s volume tolerance.” –Jude Trautlein, RD, Homemade Blended Formulas and Hydration, also from Homemade Blended Formula Handbook.
It’s very important to discuss hydration needs with your medical team. Your doctor or dietitian should be able to give an acceptable range of water needed per day based on your height, weight, age and medical conditions. Also, always monitor outputs (is the person urinating normally? How are bowel movements?).
Lastly, it’s important to remember that every body and every condition is different. Fed is best and a normal mealtime schedule might not be possible for everyone. Also, remember that illness can impact volume tolerance and even after an illness has passed, volume tolerance may not immediately go back to normal.
What’s worked for you / your loved one when it comes to volume tolerance? We’d love to hear from you on our Facebook page.