Do You Really Need a Peptide Formula?

Do You Really Need a Peptide Formula?
The basics about peptides, when they should be used, and why to consider food first
by April Jackson, MS, RD, LDN, CNSC
Even with growing support for real food for people with feeding tubes, most people with feeding tubes are still put on standard (read: cheapest!) commercial formula when they first get a feeding tube. While these formulas can literally be lifesaving, GI-related intolerance symptoms are quite common. Several studies report the incidence of GI intolerance to be as high as 75%, especially in hospitalized patients.1 2 3 These intolerance symptoms include nausea, vomiting, diarrhea, constipation, retching, and reflux.
So what’s the standard treatment when a patient is having intolerance symptoms to a regular formula? The “old way” of treating side effects looks like this:
1. Prescribe medications to treat side effects. A recent review of hospitalized patients with feeding tubes noted that more than 37.9% of patients received a medication to stimulate stomach emptying and 13.4% of patients received more than one of these medications while on tube feedings.1
The need for these medications should really be examined, especially in situations where a patient hasn’t needed them as an oral eater, but now does when fed formula-only through the tube.
2. Next, switch to a lower rate of feeding (either via gravity or pump) to treat GI intolerance symptoms related to volume intolerance or dumping syndrome.
If a person is being fed one synthetic formula as their only nutrition, and that’s causing diarrhea 50% of the time, does it make sense to keep feeding that one formula as the only source of nutrition, just slower and over more hours? Imagine giving that advice to an oral eating person!
3. Another common approach for clinicians is to switch the patient from standard formula to a peptide-based formula to see if this is better tolerated. If a peptide formula isn’t tolerated, the patient is often moved to an elemental formula.
Is the form of protein really the problem? Comparing ingredient lists of a standard formula to a peptide formula, are they really THAT different?
What Exactly is a Peptide Formula?
 The difference between standard formulas and peptide (and elemental) formulas is all about how much the protein is broken down. Peptide-based formulas, also known as semi-elemental formulas, contain partially broken down (hydrolyzed) proteins, resulting in shorter chains of amino acids. These shorter chains mimic the process that occurs during digestion of proteins in the intestines. These formulas are recommended for those experiencing malabsorption, pancreatic dysfunction, or for prolonged bowel rest following major abdominal surgery or other evidence of gastrointestinal impairment.
The difference between standard formulas and peptide (and elemental) formulas is all about how much the protein is broken down. Peptide-based formulas, also known as semi-elemental formulas, contain partially broken down (hydrolyzed) proteins, resulting in shorter chains of amino acids. These shorter chains mimic the process that occurs during digestion of proteins in the intestines. These formulas are recommended for those experiencing malabsorption, pancreatic dysfunction, or for prolonged bowel rest following major abdominal surgery or other evidence of gastrointestinal impairment.
Elemental formulas, the next step in the typical enteral formula algorithm, contain proteins that are 100% broken down into amino acids. Amino acids are the building blocks of protein that are essential for growth and development. These formulas are considered hypoallergenic and are recommended for those with milk or soy protein allergies, food protein intolerances or allergies like Eosinophilic esophagitis, and severe malabsorption.
These specialized formulas were created for people who are unable to digest real food, or with severe allergies. If the patient has eaten regular food prior to the tube being placed, or the tube was placed due to the inability to safely eat orally, do they truly need a specialized formula?
What Does the Research Say About Peptides?
Limited research exists comparing the use of standard formulas to peptide formulas, and the data is conflicting in the research that is available. Because of this, the use of peptide and elemental formulas is based on expert opinion (Grade E).5 Some evidence suggests that peptide formulas may be helpful with very specific patients, such as those with malabsorption or pancreatic dysfunction or to allow prolonged bowel rest following major abdominal surgery or other evidence of GI disease.6 However, other studies have shown little to no difference in tolerance between standard and peptide formulas.5 6 7 8.
A recent study showed improved tolerance using peptide-based diets in patients at risk for significant malabsorption because of GI surgery or pancreatitis.9 Even with this study, however, 56 percent (30/53) of patients continued to experience nausea, vomiting, diarrhea, abdominal pain/cramping, gas/bloating, and abdominal distension on the peptide-based formula. There are no known studies that compare the use of peptide formulas to a real food diet (i.e. blenderized tube feedings.)
“Overall, little evidence appears to support the routine use of elemental or peptide formulas except in the presence of GI dysfunction such as malabsorption, pancreatic dysfunction, chyle leak, or other evidence of GI disease. Elemental or peptide formulas should be reserved for patients who failed a fair trial of standard formulas.”6
Peptides vs. Whole Foods
While research comparing peptide formulas to standard formulas is limited, there is a growing body of  evidence supporting the use of blenderized diets to help improve intolerance symptoms in both adults and children. Most notable are three studies that demonstrate improved outcomes on blenderized diets when compared to conventional formulas, including patients who were previously on peptide or elemental formulas:
evidence supporting the use of blenderized diets to help improve intolerance symptoms in both adults and children. Most notable are three studies that demonstrate improved outcomes on blenderized diets when compared to conventional formulas, including patients who were previously on peptide or elemental formulas:
Efficacy and Tolerance of Blended Diets in Children Receiving Gastrostomy Feeds
In this study from Johns Hopkins, researchers focused on the prevalence of GI symptoms in children receiving a blended diet via G tube and stated, “Typically one could expect medical providers to hesitate recommending whole food-based formulas to patients receiving elemental formulas because of anticipated intolerance.”4 However, all the children in this study successfully transitioned to a blended diet, including the 65% on peptide and amino acid-based formulas. The results showed:
- 95% of patients who switched to a blenderized diet experienced improvement in GI symptoms
- 53% of patients increased their oral intake
- 2 patients were able to switch exclusively to an oral diet after switching to a blenderized diet
The authors also point out that many patients were trialed on an amino acid-based formula because of GI intolerance symptoms like reflux or vomiting, even though test results were negative for milk protein allergies. This study demonstrates that GI intolerance to formula may be alleviated with the introduction of real food and that peptide based or amino acid-based formulas are not indicated for the treatment of common GI intolerance symptoms to standard formula.
Health Outcomes and Quality of Life Indices of Children Receiving Blenderized Feeds via Enteral Tube
This study from Boston Children’s Hospital looked at health outcomes, quality of life, and healthcare usage in patients receiving blenderized feeds compared to those on conventional formula.10 Patients in the blenderized diet group had greater overall satisfaction, less stomach pain, reflux, nausea, vomiting, diarrhea, and fewer total symptoms overall. In addition, the blenderized diet group was found to have a 43% reduction in emergency room visits, a 53% reduction in hospital admissions, and a 67% reduction in respiratory related admissions. In this study, 57% of patients on conventional formula were actually on elemental diets.
Blenderized enteral nutrition diet study: Feasibility, clinical, and microbiome outcomes of providing blenderized feeds through a gastric tube in a medically complex pediatric population
Researchers at The Hospital for Sick Children reported a decrease in vomiting, gagging, retching, and use of acid suppressing medications in a medically complex pediatric population when they switched to blenderized diets. A significant number of patients in this study were on peptide and elemental formulas as well as continuous pump feeds and yet the researchers considered these patients to be appropriate candidates for blenderized diets.
When considering if a patient is a candidate for a blenderized diet, it’s important to look at the reason the tube was originally placed, not just what formula they’re currently on. Does the patient have an underlying condition necessitating the peptide or elemental formula?
In addition, these studies show that patients receiving peptide and amino acid-based formulas tolerated intact protein and had less GI intolerance when switched to a blenderized tube feeding diet consisting of whole foods.4 11
Think Food First
 While peptide formulas can be helpful for certain patients, they are often prescribed to treat common formula intolerance symptoms, and research is mixed at best at whether peptides are actually successful in helping improve these symptoms. Real food options, whether a home blenderized diet or a commercial product like Real Food Blends, should be considered first in treating intolerance symptoms before moving onto more specialized formulas. So many Real Food Blends customers have let us know over the years how real food has helped improve intolerance symptoms, helping them reduce or eliminate medications, gain weight, and be healthier overall. Now research supports what we’ve been hearing for years — that many formula intolerance symptoms improve (or are eliminated) when real food is introduced.
While peptide formulas can be helpful for certain patients, they are often prescribed to treat common formula intolerance symptoms, and research is mixed at best at whether peptides are actually successful in helping improve these symptoms. Real food options, whether a home blenderized diet or a commercial product like Real Food Blends, should be considered first in treating intolerance symptoms before moving onto more specialized formulas. So many Real Food Blends customers have let us know over the years how real food has helped improve intolerance symptoms, helping them reduce or eliminate medications, gain weight, and be healthier overall. Now research supports what we’ve been hearing for years — that many formula intolerance symptoms improve (or are eliminated) when real food is introduced.
Sources
1 Gungabissoon U, Hacquoil K, Bains C, et al. Prevalence, risk factors, clinical consequences, and treatment of enteral feed intolerance during critical illness. JPEN J Parenter Enteral Nutr. 2015;39(4):441-448. https://doi.org/10.1177/0148607114526450
2 Wang K, Mellroy K, Plank LD, et al. Prevalence, outcomes, and management of enteral tube feeding intolerance: a retrospective cohort study in a tertiary center. JPEN J Parenter Enteral Nutr. 2017;41(6):959-967. https://doi.org/10.1177/0148607115627142
3 Blaser AR, Starkopf J, Kirsimagi U, et al. Definition, prevalence, and outcome of feeding intolerance in intensive care: a systematic review and meta-analysis. Acta Anaesthesiol Scand. 2014;58(8):914-922. https://doi.org/10.1111/aas.12302
4 Batsis ID, Davis L, Prichett L, et al. Efficacy and Tolerance of Blended Diets in Children Receiving Gastrostomy Feeds. Nutr Clin Pract, 2019;00:1-7.
5 Brown B, Roehl K, Betz M. Enteral Nutrition Formula Selection: Current Evidence and Implications for Practice. Nutr Clin Pract. 2015;30(1):72-85.
6 Escuro A and Hummell AC. Enteral Formulas in Nutrition Support Practice: Is There a Better Choice for Your Patient? Nutr Clin Pract. 2016;31(6):709-722.
7 Tiengou LE, Gloro R, Pouzoulet J, et al. Semi-elemental formula or polymeric formula: is there a better choice for enteral nutrition in acute pancreatitis? Randomized comparative study. JPEN J Parenter Enteral Nutr. 2006;30(1):1-5.
8 Taylor AL, Dunstan JA, Prescott SL. Probiotic supplementation for the first 6 months of life fails to reduce the risk of atopic dermatitis and increases the risk of allergen sensitization in high-risk children; a randomized controlled trial. J Allergy Clin Immunol. 2007;119(1):184-191.
9 Mundi M, Velapati S, Kuchkuntla A, et al. Reduction in Healthcare Utilization With Transition to Peptide-Based Diets in Intolerant Home Enteral Nutrition Patients. Nutr Clin Pract. 2020;35(3):487-494.
10 Hron B, Fishman E, Lurie M, et al. Health Outcomes and Quality of Life Indices of Children Receiving Blenderized Feeds via Enteral Tube. J Pediatr. 2019;1.7.
11 Gallagher K, Flint A, Mouzaki M, et al. Blenderized Enteral Nutrition diet Study: Feasibility, Clinical, and Microbiome Outcomes of Providing Blenderized Feeds Through a Gastric Tube in a Medically Complex Pediatric Population. 2018;42(6):1046-1060.
About the author

April Jackson, MS, RD, LDN, CNSC is a Registered Dietitian with 20 years of experience in nutrition support. She is currently a Business Development Manager for Real Food Blends.
Tube Feeding and Constipation

Tube Feeding and Constipation
Preventing and treating one of the most common side effects of tube-feeding
by April Jackson, MS, RD, LDN, CNSC
Talking about bowel habits can be uncomfortable (no pun intended!), but it’s one of the most common side effects of tube-feeding. Nutrition and gut health are closely linked and you can’t really talk about bowel health without discussing the quality of your diet. It’s a fact of tube-feeding life: Regularity is something that many people with feeding tubes struggle with and it can have a direct impact on overall health and quality of life.
What is Classified as Constipation?
Constipation refers to irregularity with the number and frequency of bowel movements. Symptoms include stools that are hard, dry, and difficult to pass and can be associated with straining or pain during passage. In general, if you’re having less than 3 bowel movements per week or going more than 3 days without a bowel movement, you should discuss constipation with your medical provider.
What Causes Constipation?
In general, there are a number of causes of constipation, many of which come into play when someone with a feeding tube is fed a formula-only diet:
 1. Changes in diet. People with feeding tubes often experience a massive dietary change when going from a typical oral-eating diet to solely relying on a tube feeding formula. Many of these formulas rely on highly processed ingredients, which have been shown to lead to inflammation in the body and chronic diseases.1 2 Although infants and children who have only been formula fed may not have a sudden change in their diet, the lack of variety and progression to real food may factor into constipation issues as well. Formula-only diets lack vegetables, fruits, and whole grains – all things that would generally be encouraged to an oral-eater dealing with constipation.
1. Changes in diet. People with feeding tubes often experience a massive dietary change when going from a typical oral-eating diet to solely relying on a tube feeding formula. Many of these formulas rely on highly processed ingredients, which have been shown to lead to inflammation in the body and chronic diseases.1 2 Although infants and children who have only been formula fed may not have a sudden change in their diet, the lack of variety and progression to real food may factor into constipation issues as well. Formula-only diets lack vegetables, fruits, and whole grains – all things that would generally be encouraged to an oral-eater dealing with constipation.
2. Low fiber intake. Fiber adds bulk to stool and absorbs water from the intestines, making stools softer and easier to pass. Diets low in fiber reduce the amount of undigested food in the intestines, which leads to less stool output. Many conventional tube feeding formulas do not contain fiber or the fiber content varies greatly in type and amount. While commercial formulas with added (processed or synthetic) fiber are available, they have been shown to provide little help in treating constipation for most individuals, they increase the risk of clogging the feeding tube, and they may decrease the absorption of certain medications.3 4
3. Dehydration. Adequate fluid intake is important in maintaining regularity whether you are drinking by mouth or through your feeding tube. Fluid needs vary based on age, weight, gender, activity level, and even what climate you live in. One of the best ways to check for dehydration is urine color. The goal should be pale yellow urine.
4. Physical Limitations Decreased activity can slow down the movement of stool through the colon and causes an incomplete emptying of the bowels. This gives the body more time to absorb water out of the stool, leading to constipation. People who are bedridden or immobile typically eat less because they aren’t burning calories through activity. This also leads to longer times between bowel movements, which can also lead to constipation. People with low muscle tone, neuromuscular problems, and/or developmental delays are especially at risk of constipation.
5. Medications and supplements. Several types of medications and supplements can cause constipation. Some, like those containing aluminum and calcium, may interfere with important muscle contractions in the gut. Certain medications used to treat epilepsy, muscle spasms, and pain can also impact these muscle contractions by sending mixed signals to the gut. Diuretics can lead to dehydration (which we know is another cause of constipation). When it comes to supplements, synthetic forms of iron and zinc can lead to or exacerbate constipation, and are added to every tube-feeding formula on the market.5 [Note: Real Food Blends meals have no synthetic vitamins or minerals.]
Preventing and Relieving Constipation
If an oral-eating person complained to their doctor or medical team about constipation issues, the first questions would be: “Are you eating enough fruits and vegetables? Whole grains? Getting enough water?” Before considering adding medications for constipation, people with feeding tubes should first look at their nutrition and hydration.

Think Food First. There are a whole host of benefits from incorporating real food into your tube feeding diet. Research shows that blenderized diets can improve common GI intolerance symptoms associated with commercial formula use, including decreasing nausea and vomiting, diarrhea, reflux and constipation.2 6 7 Soluble and insoluble fibers from fruits, veggies, and whole grains have been shown to improve constipation and diarrhea in people with feeding tubes.6 2 The recommended daily intake for fiber is 14 grams per 1000 calories, which is about 25 grams per day for most women and 38 grams per day for men.1 [Each Real Food Blends meal contains 2-6 g of fiber and includes a fruit, vegetable, and whole grain or healthy starch.] Aside from the numeric fiber goals, remember that fiber quality matters! The synthetic or processed fibers added to most tube-feeding formulas may not be handled in the body the same way as the fibers from the whole foods. Just because you may be hitting a daily fiber goal from formula shouldn’t rule out that fiber still might be a contributing to constipation.
Real food can also help with constipation caused by synthetic iron supplements commonly added to formula–iron from whole food sources is generally better tolerated and results in less GI discomfort. Iron from red meat, poultry, and fish is well absorbed by the body and combining those with foods rich in vitamin C (like orange juice, kale, spinach, and sweet potatoes) increases the absorption of iron even more. [Each Real Food Blends meals contains a high quality lean protein and vitamin C rich fruits or veggies.]
Hydrate. Additional fluids are recommended with tube feedings and especially with blenderized diets, just like oral eaters are encouraged to drink eight 8 ounce glasses of water per day. These fluids can be given as additional flushes before, after, and in between feedings. [Consult your medical team for fluid recommendation for your specific needs.] Water is the typical fluid of choice, and flushing with warm liquids may help stimulate a bowel movement. (Concerned about volume intolerance? Learn more about free water and volume tolerance here.)
Using juice as an additional fluid can also help with constipation. Juices contain sorbitol, a sugar alcohol known for its natural laxative effects, and soluble fiber, which provide a fuel source for good bacteria in the gut. Prune, cherry, pear, and apple juice in particular contain high levels of sorbitol. A good starting point is flushing with 4-8 oz of prune juice daily (2-4 oz for kids) if you are experiencing constipation.8
Get moving. Increasing activity helps to speed up the movement of food through the intestines. This means that there is less time for the body to absorb fluid from the stool, making it easier to pass. Although some people with feeding tubes may be limited in the physical activity they are able to do, the Physical Guidelines for Americans state that “some physical activity is better than none, and adults who participate in any amount of physical activity gain some health benefits.”9 Consult your medical provider before starting any exercise program.
Add probiotics. Probiotics are live microorganisms that improve overall gut health. They are found in cultured or fermented foods like yogurt, kefir, cottage cheese, sauerkraut, kombucha, pickled vegetables, kimchi, miso, and tempeh. Studies suggest that L. acidophilus and B. bifidum may improve intestinal motility and relieve constipation by reducing the pH of the gut.10 Adding pourable kefir, yogurt, or cottage cheese to your tube feeding diet is an easy way to incorporate added probiotics.
This blog is not intended to be medical advice. Always consult your medical team before making any changes in your tube feeding diet.
Sources
1 U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015-2020 Dietary Guidelines for Americans. 8th ed. 2015. http://health.gov/dietaryguidelines/2015/guidelines/
2 Hron B, Fishman E, Lurie M, Clarke T, Chin Z, et al. Health Outcomes and Quality of Life Indicies of Children Receiving Blenderized Feeds via Enteral Tube. J of Peds 2019;1-7
3 Malone AM. Enteral formulations. In: Cresci GA, ed. Nutrition Suport for the Critically Ill Patient: A guide to Practice, 2nd ed. Boca Raton, FL: CRC Press; 2015:259-277.
4 Johnson T, Seegmiller S, Epp L, Mundi M. Addressing Frequent Issues of Home Enteral Nutrition Patients. Nutr in Clin Prac 2019;34:186-195.
5Tolkien Z, Stecher L, Mander A, Pereira D, et al. Ferrous Sulfate Supplementation Causes Significant Gastrointestinal Side-Effects in Adults: A Systematic Review and Meta-Analysis. PLoS One. 2015; 10(2): e0117383. Published online 2015 Feb 20.
6 Hurt, R. et al. (2015). Blenderized Tube Feeding Use in Adult Home Enteral Nutrition. Nutrition In Clinical Practice, 30, 824-9.
7Batsis ID, Davis L, Prichett L, et al. Efficacy and Tolerance of Blended Diets in Children Receiving Gastrostomy Feeds. Nutr Clin Pract, 2019;00:1-7.
8Bae S. Diets for Constipation. Pediatr Gastroenterol Hepatol Nutr. 2014 Dec; 17(4): 203–208. Published online 2014 Dec 31. doi: 10.5223/pghn.2014.17.
9U.S. Department of Health and Human Services and U.S. Department of Agriculture. Physical Activity Guidelines for Americans. 2nd Edition. 2018. Available at https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf
10 Kopp-Hoolihan L. Prophylactic and therapeutic uses of probiotics: A review. Journal of The American Dietetic Association 2001;101:229-241
About the author

April Jackson, MS, RD, LDN, CNSC is a Registered Dietitian with 20 years of experience in nutrition support. She is currently a Business Development Manager for Real Food Blends.
The Role of Real Food in Tube Weaning

The Role of Real Food in Tube Weaning
Research supports increased interest in oral eating with blenderized diets

“My child is now eating Real Food Blends orally!”
This is a comment we get quite a bit and might be one of our very favorite “side effects” of using Real Food Blends in place of a typical tube-feeding formula. Aside from the anecdotal evidence we hear time and again, many of the studies about real food for people with feeding tubes note this “increased interest in oral eating.” Below, Aubrey Phelps, MS, RDN, PPCES, IFNCP, goes over different studies that show how using real food can help facilitate the transition to eating orally and what the results mean outside of a clinical setting. She also has personal experience with this topic—her daughter was able to transition from using Real Food Blends with her feeding tube to 100% oral eating!
by Aubrey Phelps, MS RDN, PPCES, IFNCP
Getting your child with a feeding tube to happily become an oral eater can seem like a monumental task. There are many factors that go into a successful tube-wean, but one often-overlooked aspect to tube-weaning is that introducing food through the tube prior to starting a wean can increase the chances of success. Aside from anecdotal evidence (including my own daughter!), two independent research studies have noted this impact:
“The parents of 17 of 33 children (52%) reported a 76% to 100% decrease in gagging and retching after their child started the PBGT diet… No parents reported that their child’s gagging or retching worsened on the PBGT diet”
“Nineteen children (57%) were reported to have an increase in oral intake on the pureed by gastrostomy tube (PBGT) diet… No child was reported to eat less by mouth after starting the PBGT diet”
“The decrease in gagging and retching on puréed feeds may have decreased oral aversion, making the child more receptive to eating by mouth”
Puree by gastrostomy tube diet improves gagging and retching in children with fundoplication
Pentiuk et al (2011) – Cincinnati Children’s Hospital Medical Center
This study looked at the use of purees through the g-tube, specifically for kids. To summarize the key take-aways quoted above, switching to a pureed real food diet improved reflux and retching in over half of the kids—this is one of the most common reported frustrations of parents with children using a tube and a prime reason for a switch to a J-tube. For that group, improvement was significant, ranging from almost completely stopping reflux and retching to being totally eliminated. And none of the kids had worsened symptoms when they switched. In other words, there’s a great chance switching to a blenderized/real food puree diet could improve your child’s vomiting and gagging and very little chance it could make things any worse (so you don’t really have anything to lose!).
This study also concluded that oral intake improved with a pureed tube-fed diet and that this improvement was likely thanks to the reduction in digestive discomfort. Because oral aversions are a huge contributor to tube-feeding and an obstacle to improving oral intake for a wean, this approach to tube-feeding may help lead the way to weaning or increasing oral intake as appropriate to the individual’s medical needs.
“Parents reported less limitation to food and drink intake with blenderized diets. This may reflect improved gastrointestinal tolerance of dietary components, increased perception of diversity of diet, or increased oral intake, as suggested by Gallagher et al”

Health outcomes and quality of life indices of children receiving blenderized feeds via enteral tube
Horn et al (2019) – Boston Children’s Hospital
And yet again, this study found that kids simply did better on blenderized diets, from a comfort standpoint, as well as oral intake. (If you are on the fence about trailing a blended diet like Real Food Blends, I would highly encourage you to read this entire study. It’s the largest done to date on blended diets and is a head-to-head comparison of formula-fed children to children fed real food. No surprise, those getting a wide variety of fruits & veggies fared much better!)
Why Does Real Food Often Increase Interest in Oral Eating?
Exactly why getting a variety of real food into the stomach through the tube seems to create this willingness to eat orally is debated. Improvements in reflux, vomiting, constipation/diarrhea, and lowering or eliminating medications to manage all these symptoms can all contribute to increased in eating orally. After all, who would want to eat if they feel sick or uncomfortable all the time?
It could also be from improvements in the gut microbiome, as one of the studies above supported. Each type of bacteria in your gut has a preference for certain kinds of foods–the “good guys” really, really like fiber, fruits, and vegetables. A real food diet encourages the growth of more of these good bacteria, which in turn, encourages a desire for more of the food that they like! Less healthy microbes prefer processed carbs/sugars, which most commercial tube-feeding formulas are quite high in. Improvement in microbiome balance also supports a happier digestive system, which can improve both digestion and immune health (and doesn’t it make sense that a kid who’s no longer sick all the time might have more interest in eating?). It’s important to note that in all these studies, the children were fed a varied, whole food diet exposing their bodies to a wide variety of food, smells, and ‘tastes.’
With all of these potential gains, there are really no reasons to NOT trial a blenderized diet like Real Food Blends if your child is over the age of 1 and has an intact and working digestive system. Even if it doesn’t increase oral intake, it will likely improve digestive comfort and will have a positive impact on the microbiome, which supports overall improved health! (And there’s a growing body of clinical support from major medical institutions showing that real food is good for kids – go figure!)
About the author

Aubrey Phelps, MS, RDN, PPCES, IFNCP is a registered integrative nutritionist specializing in perinatal and pediatric nutrition. She’s a momma to a former tubie who thrived on Real Food Blends before she weaned to a diverse, real food oral diet! Outside of her private practice, Aubrey consults for Growing Independent Eaters, a home-based tube-weaning program, as well as Real Food Blends.
Additional Information on Tube Weaning
Learn more about how real food through the feeding tube can help with the tube weaning process in this video from Marsha Dunn Klein, a pediatric occupational therapist who has spent a career specializing in pediatric feeding challenges.

Listen to our co-founder, Julie Bombacino, talk about the role of real food in tube weaning on the Tube to Table podcast from Thrive by Spectrum Pediatrics.
The Value of Daily Values
The Value of Daily Values?
What’s really behind all those nutrition numbers
by Sarah Kiser, MS, RD, CSO, CNSC
There are many terms to describe “nutrient needs.” DRIs, RDIs, RDAs, DRVs, ABC123s (just kidding on that last one), but what do they all mean? What do they mean for people with feeding tubes?
In the feeding tube world, the phrase “nutritionally complete” gets used a lot, but it’s important to know that formulas are made nutritionally complete with the use of supplements. (Read “The Facts About ‘Nutritionally Complete” here.) First, we need to get into some definitions. There are two general classes of analyzing nutrient needs: Daily Values (DVs) and Dietary Reference Intakes (DRIs). They overlap and are sometimes used interchangeably, but it is helpful to know where the differences lie.
Daily Values (DVs)
DVs are reference amounts of nutrients to consume. These are the percentages you see listed on the Nutrition Facts panel on food labels. DVs are based on two things:
- Reference Daily Intakes (RDIs): a set of references for vitamins and minerals on food labels based on recommended dietary allowances (RDAs)
- Daily Reference Values (DRVs): these are established for fat, saturated fat, cholesterol, carbohydrates, protein, dietary fiber, sodium, and potassium
RDIs typically represent the recommended nutrients of the group with the highest need. For example, the RDI for vitamin D is 20 mcg, which is the RDA for adults over the age of 70. Meanwhile, the RDI for calcium is 1300 mg, which is the RDA for children 9-18 years of age. These age groups have the highest need for vitamin D and calcium, respectively. That means the DV does not represent the much wider population which typically doesn’t need as much vitamin D and calcium. These reference values listed on food labels simply provide context for consumers to know what they are eating and are intended to cover the widest group of people possible.
DVs are:
- Used on food labels
- Provide perspective on daily nutrient needs for adults and children ages 4 and up
- Based on a 2,000-calorie diet
DVs are not:
- Recommended intakes for individuals
- Age, gender, or life stage specific
- Always applicable to those who need less or greater than 2,000 calories daily
Dietary Reference Intakes (DRIs)
In contrast to RDIs, DRIs do vary by age, gender, and life stage. DRIs are used to determine nutrient needs for healthy people. The most important terms to know related to DRIs are:
- Recommended Dietary Allowance (RDA): The average daily level of intake that meets the nutrient requirements of 97-98% of healthy people;
- Adequate Intake (AI): established when there isn’t enough data to create an RDA. This is set at a level assumed to ensure nutritional adequacy for healthy people.
RDAs are broken out by age and gender with predetermined heights and weights. These reference weight-and-height values are not necessarily ideal; they simply make it possible to define recommended nutrient intakes appropriate for the largest number of people. RDAs meet or exceed the actual requirements of all but 2-3% of the population. Some people may not meet RDAs with their daily diets but may still meet their individual requirements.
While DRIs are more age, gender, and life stage specific than DVs, DVs are used on food labels and many enteral formula labels. Remember, DVs only provide information on daily nutrient needs for people 4 years old and older and are not recommended intakes for individuals.
One thing that DVs and DRIs share in common? They are both created for healthy people. People with feeding tubes fall across the spectrum of “health” and often have more unique needs to consider. A child with failure to thrive or an adult with severe muscle wasting probably do not fall into the reference weight-for-height values used to determine RDAs.
DRIs and DVs are certainly useful in serving as a benchmark for nutrient needs. But for people with feeding tubes especially, it is important to remember that the DVs shown on many formula labels aren’t necessarily accurate for your specific needs. When determining nutrient needs for an individual person, it is important to consider that their specific medical diagnoses, medications, weight and weight changes, and symptoms of nutrient deficiencies.
Food or Supplements?

The Dietary Guidelines for Americans state that your nutritional needs should be primarily met through a variety of nutrient-dense foods across all food groups. The American Institute for Cancer Research recommends that most people aim to meet nutritional needs through a healthy, varied diet alone, and cautions against using dietary supplements to decrease cancer risk.
Supplements are not intended to substitute for food and cannot duplicate all of the benefits from whole foods. Beyond vitamins and minerals, whole foods contain thousands of important nutrients, like carotenoids, flavonoids, and other antioxidants and phytochemicals that are not found in supplements. Many of these nutrients work together to enhance absorption and reduce risk for chronic disease, and supplements do not replicate the synergistic effects of nutrients in real food.
The evidence supporting the benefits of multivitamin and nutrient supplements is mixed. While it may seem that dietary supplements are all innocuous, it is important to remember that this is not the case. For example, high-dose beta-carotene supplements have been linked to an increased risk for lung cancer in current and former smokers.
Some populations may benefit from vitamin and/or mineral supplements added to a whole food, varied diet. It is always recommended that you consult with your registered dietitian or physician to evaluate your individual nutrient and supplement needs, whether you eat through a feeding tube or mouth!
The bottom line is: food first, supplements second – if necessary.
What Does This All Mean for Tube-Feeding?

The Real Food Blends Difference
Real Food Blends is the only line of tube-feeding formula that truly replicates a whole food, varied diet that is universally recommended for good health – without added synthetic vitamins or minerals. Real Food Blends meals feature:
- Only 5-7 real food ingredients.
- No added sugar, preservatives, or additives.
- Free from gluten, soy, nuts, and dairy.
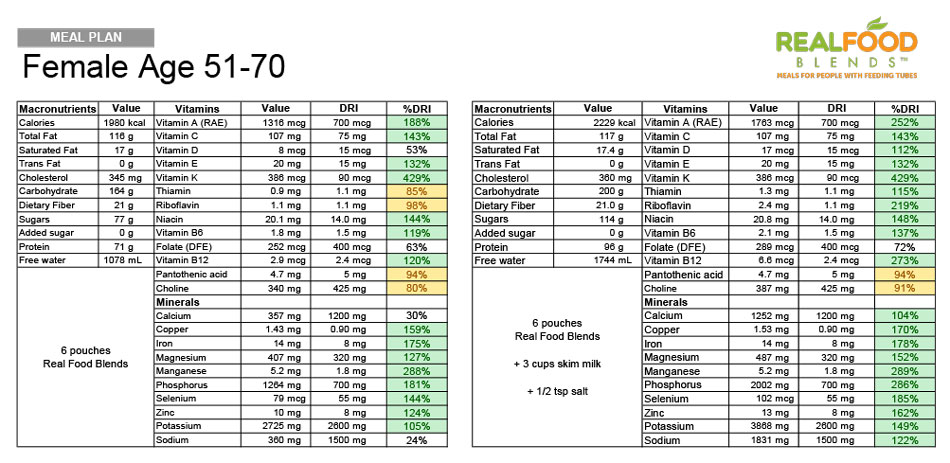
Check out how our meals compare to the DRIs for different age ranges without adding in synthetic vitamins or minerals. When used as a primary source of nutrition, we recommend adding dairy (pourable Kefir is one of our favorites for the Calcium and probiotics) or a non-dairy substitute to round out calcium and vitamin D intake, as well as a source of sodium, like salt or broth. Remember, individual needs may differ from the DVs and DRIs, but in general, most dietitians agree that it’s better to eat an orange than take a Vitamin C supplement and hitting these goals every day shouldn’t be at the expense of the basics of good nutrition (i.e. avoiding added sugars, processed foods, eating a wide variety of whole foods, etc.)
Sarah Kiser, MS, RD, CSO, CNSC is a Business Development Manager for Real Food Blends and has more than 6 years of experience as an oncology dietitian and working with home healthcare companies.
Getting Started with Real Food Blends

Getting Started With Real Food Blends
Tips for transitioning from formula
The information below is not medical advice. Always work with your medical team before making any changes to your enteral nutrition, especially if you have never consumed real food before or have reason to suspect allergies. Keep in mind that one Real Food Blends meal equals 8 ounces (one typical can of formula).
Seven day sample schedule for getting more out of real food
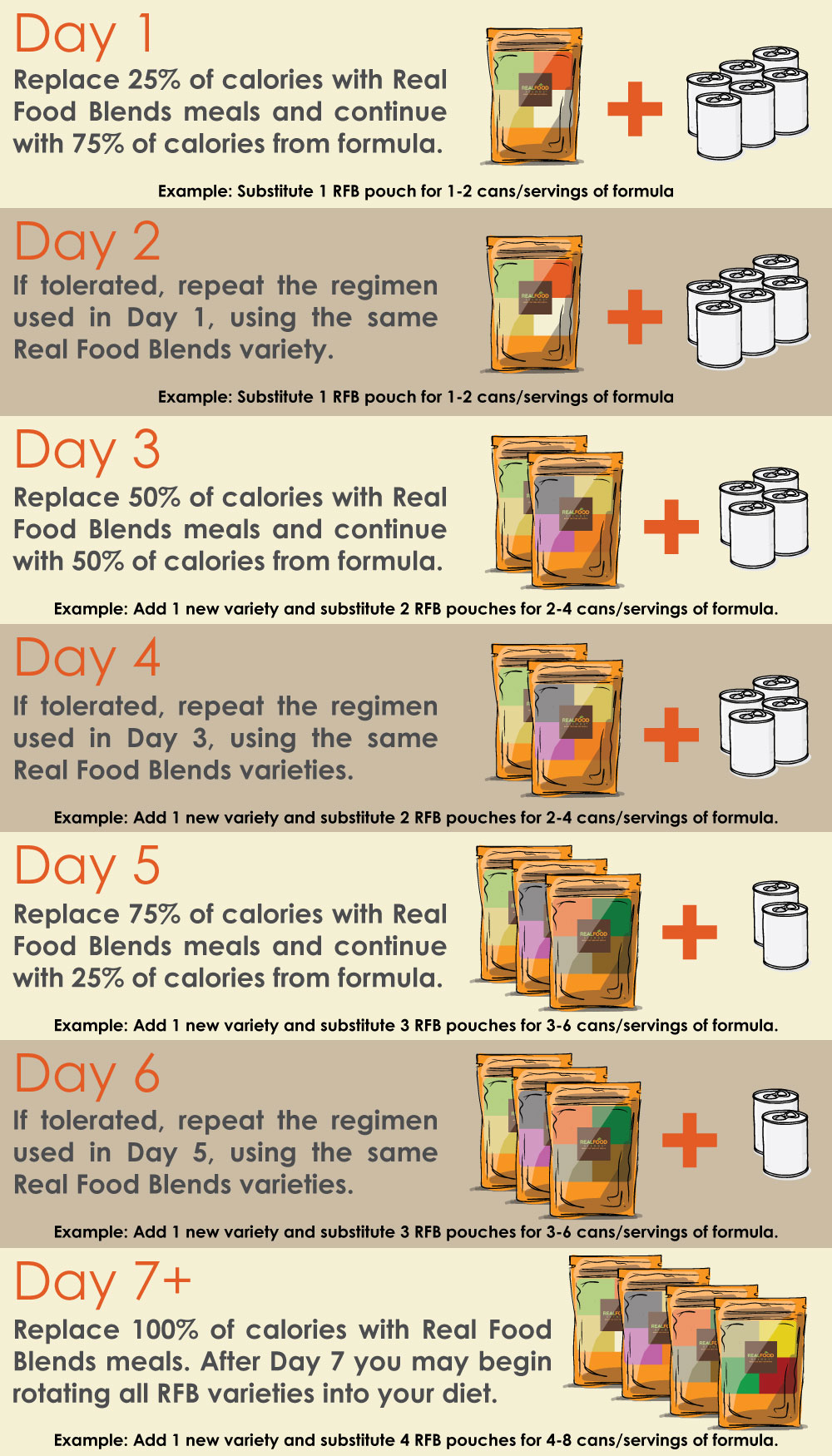
- The number of Real Food Blends pouches you will need per day will vary based on your daily caloric goal set by your medical team. Don’t be surprised if you need more calories from real food than you required on formula – this is common and luckily volume tolerance tends to increase with real food as well to help make hitting those goals easier!
- Whenever possible, we like to encourage working toward a normal mealtime schedule of breakfast, lunch, and dinner (with maybe a snack or two thrown in for extra calories), versus continuous or overnight feeds. If you have been on continuous feeds, it may take some time to get toward this schedule, but often this can be done once the body adjusts to having real food again.
- We like to encourage the use of the slow-push bolus feeding method with a syringe to keep our meals as thick as possible. The thickness tends to help with reflux symptoms and can provide a feeling of satisfaction that a pure liquid meal doesn’t always provide. When you are transitioning, though, you might find it easier to mix the meals with some formula or water for a thinner consistency or to feed through a pump or gravity bag. That’s okay! The point is to start getting some real food into the body and you can slowly head toward bolus feeding when ready.
- After day 7, ideally you would introduce the other two RFB varieties into your diet and continue to rotate the meals. For even more variety, consider some simple additions like whole milk or pourable Kefir for added calcium. Our Real Food Blends recipe book has more ideas too!
How to Use Real Food Blends
Adding to Real Food Blends Meals
Additional Tips
- Add water to meet hydration needs – same as oral eaters do! Discuss with your medical team about how much water is needed and also take note of outputs. In general, urine should be pale yellow and stools easy to pass. Additional water may be necessary in hot weather and/or when ill.
- RFB meals contain no added sodium. If you’re not on a sodium restricted diet, adding anywhere from ¼ to 1 teaspoon of salt per day would meet your daily sodium requirements (depending on your age and weight). Always consult with your medical team on exact needs.
- RFB meals contain no added synthetic vitamins or minerals. You may want to consider adding an age-appropriate multi-vitamin along with a calcium supplement to meet your nutritional needs once fully transitioned to RFB.
- If a thinner consistency is required, add water/fluid to the pouch via syringe. Warming can also help thin the meals if desired.
- Knead the meal before opening the package to improve consistency, especially if the meal has been exposed to colder temperatures.
How to Administer Real Food Blends Using Bolus Method
Step 1: Open Pouch

Step 2: Insert Syringe & Draw

Step 3: Slow Push to Administer